September 10, 2024
Anxiety Urinary Incontinence: Reasons, Signs And Symptoms And Treatment
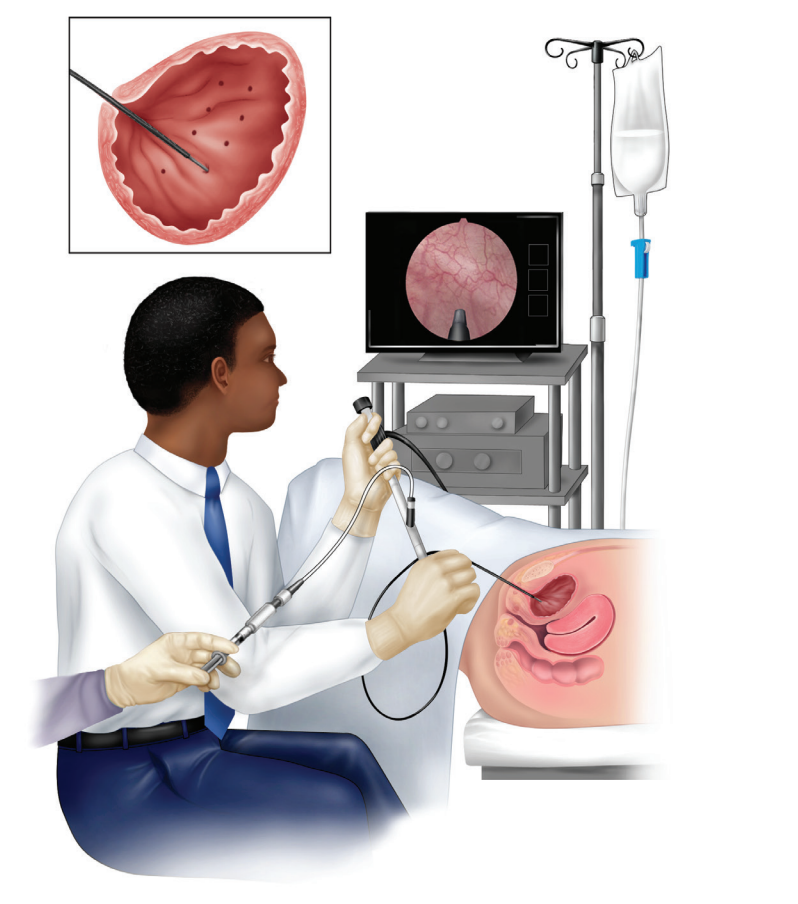
Management Of Urinary Incontinence In Postmenopausal Females: An Emas Scientific Overview Throughout a female's life, from puberty to menopause, the delicate equilibrium of hormones orchestrates a symphony of changes that can affect urinary system continence and pelvic floor stamina. Occasionally, there are changes to your everyday life that can in fact help your incontinence. These adjustments usually include workouts you can do to strengthen your pelvic floor muscular tissues, changes to your regular practices and a boosted diet plan. Some people notice improvements by making these modifications at home and don't need added treatment. 1) Urodynamic test where pressures of bladder and urethra are measured. It does not seem that the very first cause of dystrophy or cancer of exterior genitalia is estrogen deprivation. Hit to vaginal might be accountable for about 15 percent of bleeding after menopause, and on the other hand, the incidence of Vaginitis over the years after menopause boosts. Some think that specific children create a pattern of not kicking back the pelvic flooring while invalidating. In some cases, this can be traced back to an infection or a few other poisonous stimuli. A vicious circle of pelvic flooring convulsion, irregular bowel movements, and urinary system retention can create.Impulse Incontinence Pathophysiology
These hormonal changes can affect bladder function and urinary habits, https://s3.us-east-2.amazonaws.com/075ixjw8vbirserw/Urinary-health/urinary-retention/overactive-bladder-at-night-treatment-and.html manifesting as urinary system signs such as enhanced regularity, urgency, or leak. Low levels of estrogen and urinary incontinence go together. As ladies age and start coming close to menopause, the ovaries reduce the procedure of making estrogen, and the degrees of this women sex hormone naturally decrease in the body. [newline] Ultimately, with menopause, the manufacturing of estrogen quits, and this affects the body in lots of methods. Without estrogen, women find it hard to preserve healthy and balanced urologic features during and after menopause. Bladder control for ladies begins alongside their final menstrual duration and raises thereafter.Neurologic Reasons
Urethral incompetence typically leads to recurring urinary incontinence, normally at remainder. Hormone treatment (estrogen) in postmenopausal females reduces urinary regularity which results in enhance in the stamina of muscle mass around the bladder. Althoughbasic science in this field is limited, a current placebo-controlled, randomizedclinical trial of estrogen alone clarifies this issue. Urethral closureis dependent on the integrated activity of the suburethral vaginal wall, thepubourethral ligaments, the pubococcygeus muscles, and the paraurethral connectivetissues. As you age, the muscles that support your pelvic body organs can compromise. This indicates that your bladder and urethra have much less assistance-- often leading to urine leakage.Treatment For Low Estrogen Bladder Signs
Serious negative effects from imipramine are unusual yet can consist of heart and capillary problems. They might include an uneven heart beat and wooziness or fainting from reduced high blood pressure when you stand up promptly. Children and older adults may be particularly in jeopardy of these adverse effects. Give your health care service provider a full listing of your drugs before you start taking this drug.- When it involves sexual and reproductive health, it can be difficult to know what's "normal" and what may suggest a potential illness.
- The major cause of stress and anxiety incontinence is urethral hypermobility as a result of damaged assistance from pelvic flooring.
- That based on the topic of this short article, a number is mentioned.
- While in your home, your service provider might recommend you keep track of any type of leak in a journal for a couple of days.
- An extended-release form taken once daily could trigger less negative effects.
Is urinary system bladder under hormonal control?
:max_bytes(150000):strip_icc()/GettyImages-1156991077-63abeae534eb4abb88a83863c8c11928.jpg )

Social Links