September 12, 2024
6 Ways To Deal With Bladder Leakage
The Influence Of Hormone Therapy On Urinary Incontinence Incontinence Institute It can additionally compromise your pelvic flooring muscles, making it tougher to hold in pee. Nonneurogenic urinary incontinence may be caused by anatomic or practical disorders (e.g., ectopic ureters) impacting the storage space stage of micturition. Hormone-responsive urinary incontinence is likewise a typical type of nonneurogenic urinary incontinence. In these clients (generally pets), the detrusor response is normal; regular urination habits, along with pee dribbling, takes place.What Is The Difference Between Stress Urinary Incontinence And Prompt Incontinence?
Why do I leakage pee after my duration?
- Hormonal agents influence hair's all-natural cycle and structure.Skin problems.Sex-related symptoms.Weight changes.Mood and sleep issues.Digestive distress. Hormone control or contraception medication.Hormone substitute medications.Anti-androgen medications.Vaginal estrogen.Clomiphene and letrozole.Assisted reproductive
- technology.Metformin.Levothyroxine. Antidiuretic hormonal agent('ADH)is a chemical generated in the brain that triggers the kidneys to release less water, lowering the quantity of urine created. A high ADH degree causes the body to create less urine.

News From Mayo Center
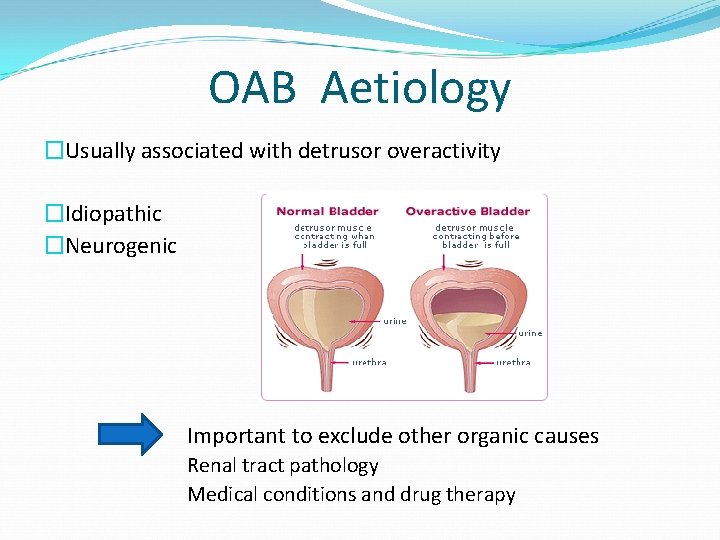
Your bladder resembles a tank-- as soon as the bladder is full, the brain sends a signal that it's time to urinate. Urine after that leaves the bladder when a muscle opens up (sphincter), enabling the urine to stream easily out of the body with the urethra. It is necessary to establish the sort of urinary incontinence that you have, and your signs often inform your medical professional which type you have. During this procedure, the posterior wall surface of the urethra shears off the anterior urethral wall surface to open the bladder neck when innate sphincter deficiency is present. Functional urinary incontinence is the lack of ability to hold urine as a result of factors other than neuro-urologic and reduced urinary system system disorder. Videourodynamic studies are reserved to assess complicated instances of stress and anxiety urinary incontinence. The therapy leading to lower testosterone levels can compromise the pelvic floor muscles, causing UI. Consequently, interventions such as pelvic exercises might be essential in taking care of UI if you are getting ADT. Additionally stop the flow of pee in midstream pee triggers to reinforce the pelvic floor muscles. Most females experience premenstrual disorder (PMS) concerning 1-2 weeks prior to bleeding begins. An alternative strategy that utilizes drug, lifestyle changes, https://seoneodev.blob.core.windows.net/health-nutrition/treatment-options/bladder-infection/the-effect-of-hormonal-agent-therapy-on-urinary-system-incontinence-urinary.html physical therapy, or various other interventions may help reduce them or help someone handle them. Many individuals believe that it's something that simply supports aging and is an inescapable concern. If you locate that incontinence is troubling your daily activities and triggering you to lose out on things you usually delight in, speak to your doctor.- Refined blockage and the results of aging on smooth muscle mass and the autonomic nerves are 2 possible contributors.
- If you have a chronic problem like diabetes mellitus or multiple sclerosis, you may have urinary incontinence for a. extended period of time.
- The suggested dosage is 1.5 to 2.0 mg/kg two times daily to three times daily.
- Occasionally it is the initial and only sign of an urinary tract infection.
Social Links